On This Page
Claims
To increase the speed and accuracy with which your claims are processed, we recommend filing claims via Electronic Data Interchange (EDI). To get started, please review the Electronic Data Interchange (EDI) section.
University of Utah Health Plans Trading Partner Setup and EFT Enrollment (835,837)
Submit Claims
If electronic submission is not an option at this time, submit CMS-1500 or UB-04 claim forms to the following address:
University of Utah Health Plans
Attention: Claims Department
PO Box 45180
Salt Lake City, UT 84145-0180
Check Claims Status Online
Wondering if a claim was received? Finished processing? What was paid to the provider, or what is the member's responsibility? Save yourself a phone call by checking the claims status online.
- Contracted providers with a secure account – View claims status via our Provider Portal
- Noncontracted providers or contracted providers waiting for their Provider Portal account to be set up, contact our Customer Service team:
Hours: M–F, 7 am–7 pm
Phone: 833-981-0213
Contact Us
If you have any additional questions, feel free to contact us:
Hours: M–F, 7 am–7 pm
Phone: 833-981-0213
Electronic Data Interchange (EDI)
Why EDI?
Electronic Data Interchange (EDI) offers significant benefits for both providers and payers. Electronic claims can help improve efficiency, productivity, and cash flow for providers, while payers can see benefits in the reduction of data entry errors and faster turnaround times.
Of the claims that University of Utah Health Plans (U of U Health Plans) receives electronically, 80% pass through our claims processing system without processor intervention. The average turnaround time for EDI claims (from the received date to the check being received in the provider's office) is 15 days.
Forms
EDI Form for 835, 837 (Trading Partner Setup) & EFT Enrollment (Electronic Funds Transfer)
- Electronic Form: UUHP EDI Enrollment
- Printable Form: PDF Form
Accepted Transactions
UUHP is currently accepting the following HIPAA-compliant transactions:
- 837 005010X224 (Dental)
- 837 005010X222A1 (Professional claims)
- 837 005010X223A2 (Institutional claims)
- 277CA Claim Acknowledgment/error report
- 999 Acknowledgement
- 835 005010X221A1 (Remittance advice)
- EFT (Electronic funds transfer) in conjunction with the 835
- COB (Coordination of Benefits)
- 270/271 0051010X279A1 Eligibility Request/Response (real time)
- 276/277 Claim status inquiry/response (real-time)
If EDI Connection issues occur during off hours for real-time 270/271 and 276/277 transactions, please contact the U of U Help Desk at 801-587-6000.
In compliance with CORE requirement 270, U of U Health Plans uses the UHIN clearinghouse for all EDI transactions. Please view the UHIN Connectivity Companion Guide for further instructions. Connectivity Companion Guide can be located at www.uhin.org
Utah Health Information Network (UHIN)
U of U Health Plans is a member of the Utah Health Information Network (UHIN), a non-profit coalition of payers and providers in Utah. UHIN members have come together to reduce the administrative costs of health care through the standardization of electronic interactions.
For more information about UHIN, visit their website: www.uhin.org
UUHP’s trading partner number with UHIN is HT000179-002.
Utah Health Information Network (UHIN)
All HIPAA-compliant transactions with University of Utah Health Plans must be submitted through the Utah Health Information Network (UHIN).
Trading Partner Registration
*If currently submitting through a clearinghouse, it is not necessary to register with UHIN. Established clearinghouses already have a trading partner number set up to submit electronic transactions through UHIN to Utah payers.
If you are not submitting your claims through a clearinghouse, you can obtain a trading partner ID through UHIN. UHIN offers all HIPAA-compliant transactions. Go to https://uhin.org/new-account-setup to start the enrollment process. Follow the steps listed on the website.
EDI Enrollment Process for the 835 and EFT
Please start ERA enrollment through your clearinghouse. They will then submit the form to U of U Health Plans on your behalf.
A Provider must be enrolled with the 837 to receive the 835 and EFT transaction. The 835 and EFT transactions are linked together by the Billing Provider NPI, and a Provider must enroll in both transactions. To receive the 835 a provider must be enrolled with the EFT, and to receive the EFT a provider must be enrolled with the 835.
Once UUHP receives the EDI Enrollment form, it will begin setting up the EDI connections. The provider will be notified by email once the setup is complete.
Questions?
Any EDI enrollment questions can be sent to uuhpedi@hsc.utah.edu
Submitting Claims
EDI Enrollment Process for the 835 and EFT
There are several different options for submitting claims to U of U Health Plans. These include the following:
- MyUHIN - Through UHIN directly to send claims and retrieve all acknowledgment reports and remittance advice.
- Clearinghouses - UHIN has a connection to most national clearinghouses and supports all HIPAA-compliant billing software.
UHIN Contracted Clearinghouses
A partial list of UHIN contracted clearinghouses appears below:
Please Note: The clearinghouse assigns Payer ID numbers. University of Utah Health Plans does not assign or maintain these numbers; please contact your clearinghouse for this information.
Hours & Schedule
Claims can be submitted 24/7.
UHIN Customer Service: (877) 693-3071
Hours: Mon – Fri: 8 a.m. – 12 p.m. | 1 p.m. – 4 p.m. MT with 24/7 emergency support
EDI Support:
Phone: (801) 587-2638 or (801) 587-2639
Fax: (801) 281-6121
Email: uuhpedi@hsc.utah.edu
Tips for Submitting Claims
Corrected Claims:
U of U Health Plans can accept corrected claims by EDI and prefers to receive claims in this format.
- Claim Header Level: Place a code 7 in the CLM05-3 segment (see 5010 Implementation Guides on Claim Frequency Type Code, page 161)
- Please include the original claim number being corrected.
Notes:
Claim notes, claim line notes (professional claims only), and claim billing notes (institutional claims only) can be submitted in the electronic file. U of U Health Plans will not know if the claim note(s) affect the claim payment; therefore, U of U Health Plans will pend any claims with claim notes for review. If the notes you are submitting do not affect claim payment, the claims will take longer to process as they will require manual review, so we ask that you limit claim notes to only information such as:
- Accident details
- Auto or subrogation detail
- Any special circumstances
You can find more information about claims and claim line notes on pages 211 and 415 of the Professional Implementation Guide. You can find more information about claim notes and claim billing notes on pages 180 and 182 of the Institutional Implementation Guide.
Identifying Members
The following information describes how to identify members of University of Utah Health Insurance Plans. There are three ways to verify University of Utah Health Insurance Plan members:
- Log in to the secure Provider Portal (Don't have a Provider Portal account? Steps follow below)
- Check Member ID cards
- Contact support
Provider Portal
Contracted providers are strongly encouraged to create a Provider Portal Account.
Use the Provider Portal to verify eligibility, review member benefits, process claims, and request prior authorizations.
Member ID cards
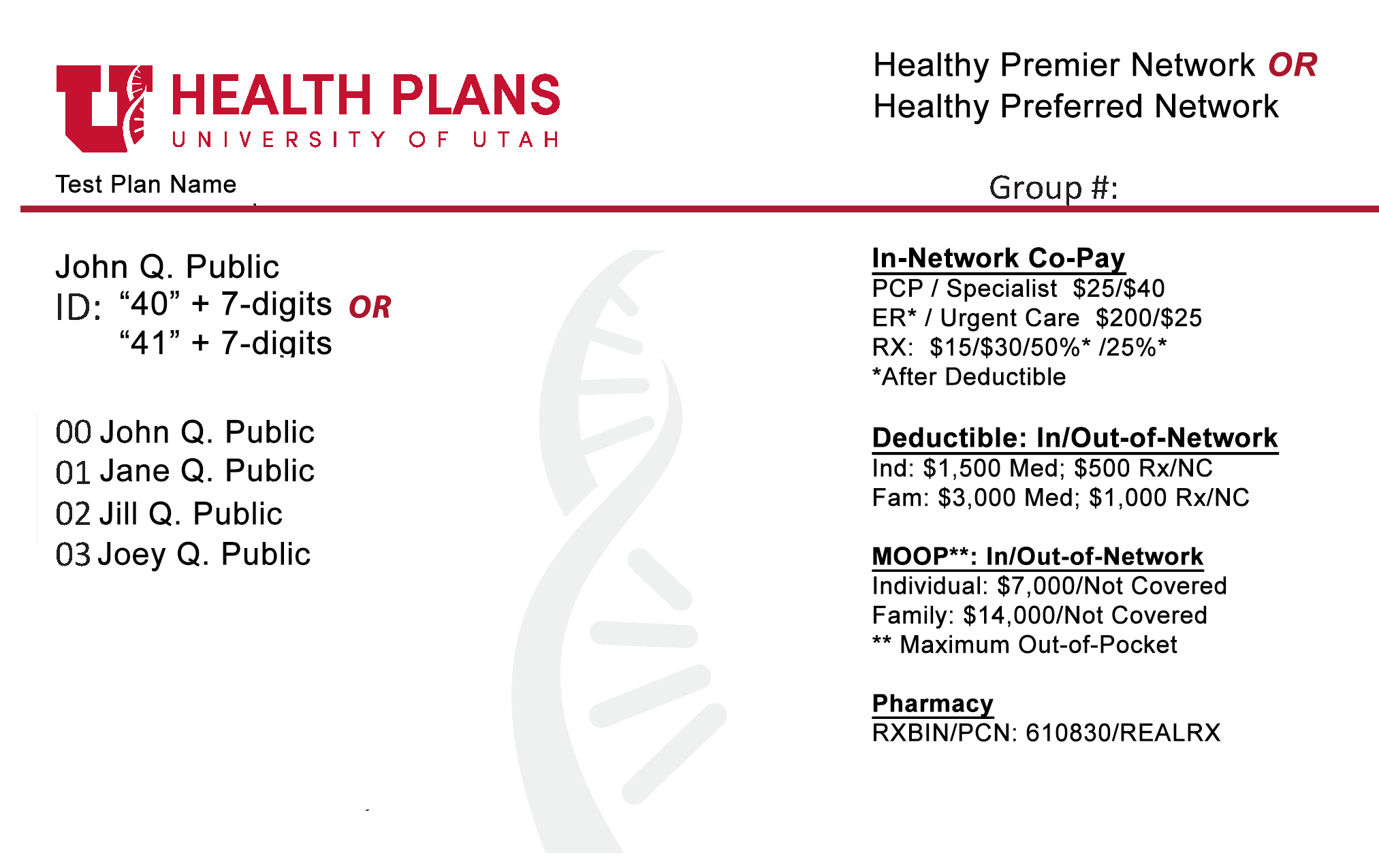
Group/Employers
The group's plan Name. Typically, the employer's company name.
Member ID numbers consist of a '40' or '41', followed by an additional seven (7) digits.
Healthy Preferred or Healthy Premier. The Healthy Preferred network is available to employer groups along the Wasatch Front. The Healthy Premier network is available to groups throughout Utah and surrounding areas.
The Group # identifies the employer or group under which the policy is issued
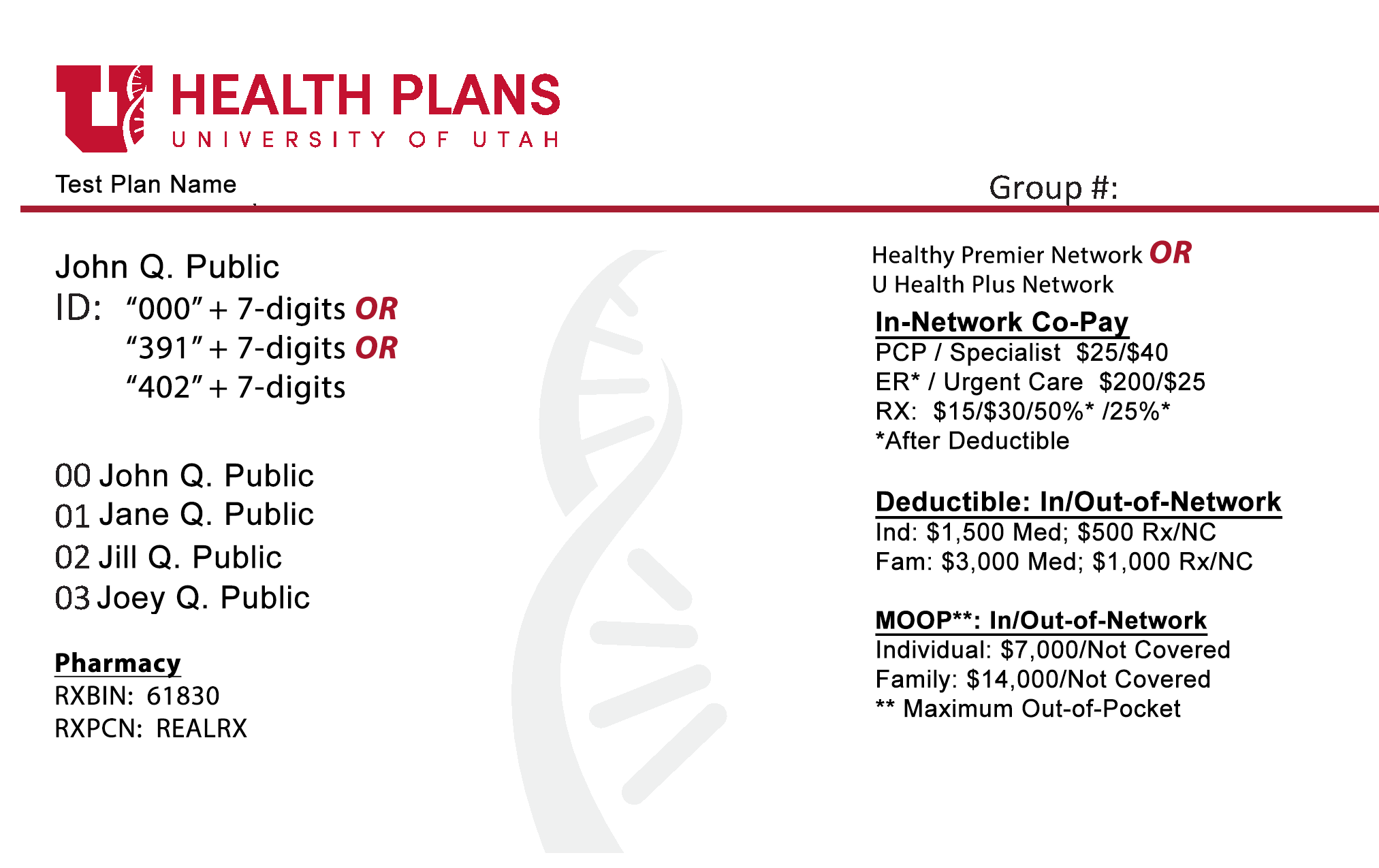
Individual/Family
The group's plan Name. Typically, the employer's company name.
Individual or Family plans may be purchased on or off the federal Health Insurance Marketplace. Member ID numbers consist of '000', '391' or '402', followed by an additional seven (7) digits.
Healthy Premier or U Health Plus. The Healthy Premier network is available to groups throughout Utah and surrounding areas. U Health Plus plans are available for Individual and Family plan members presiding in Salt Lake (except zipcode 84006) or Davis county.
The Group # identifies the group under which the policy is issued
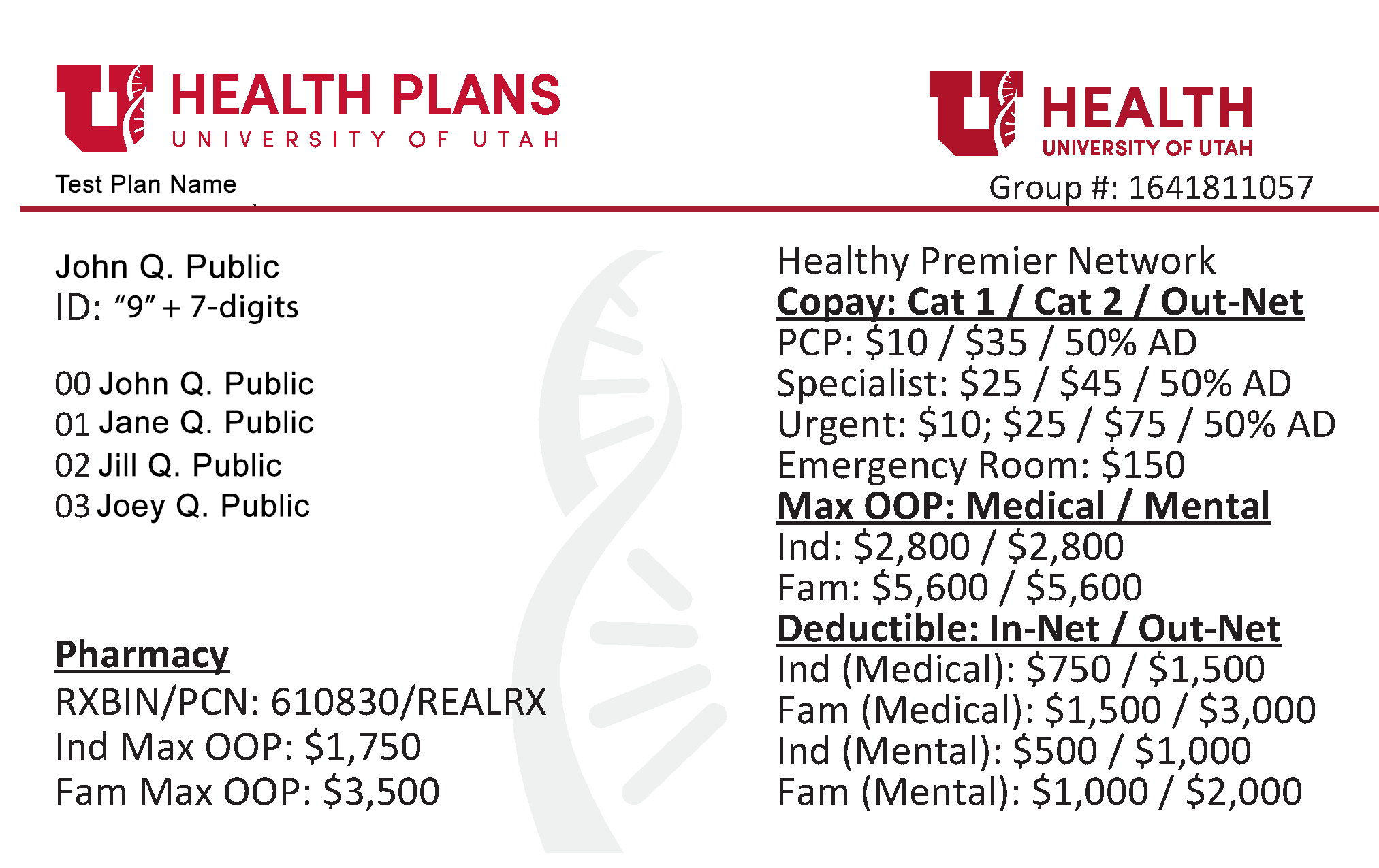
University of Utah Hospitals & Clinics
The group's plan Name (U Health Hospital).
Member ID numbers consist of a '9' followed by an additional seven (7) digits.
The Healthy Premier University of Utah Hospitals & Clinics plan is available to U of U Health employees. The Healthy Premier network is available to groups throughout Utah and surrounding areas.
The Group # identifies the employer or group under which the policy is issued
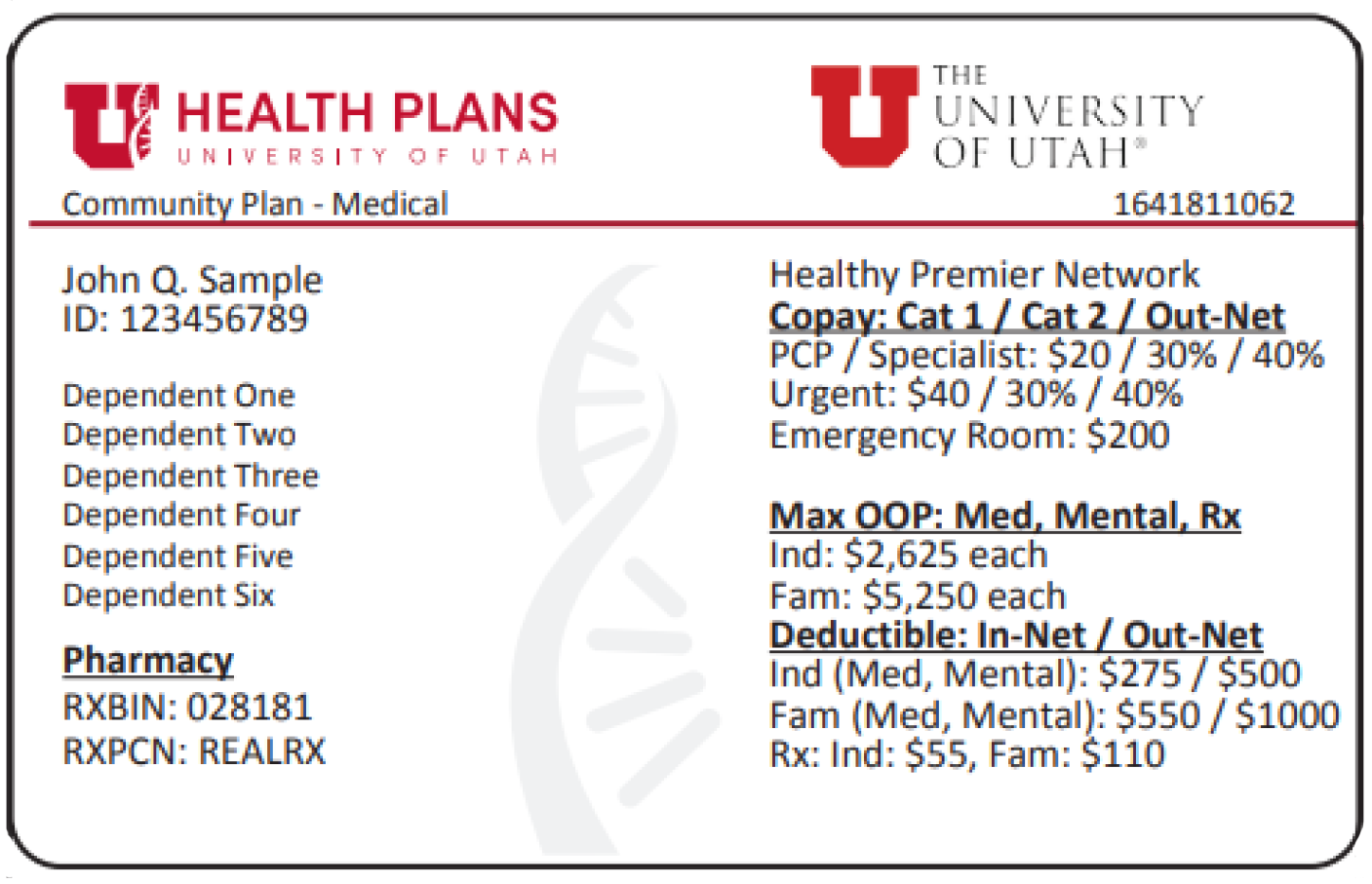
University of Utah Community Plan
The group's plan name "Community Plan - Medical" or "Community Plan - Medical & Dental".
Member ID numbers consist of a '9' followed by an additional seven (7) digits.
The Healthy Premier University of Utah Community plan is available to U of U Campus employees. The Healthy Premier network is available to groups throughout Utah and surrounding areas.
The Group # identifies the employer or group under which the policy is issued
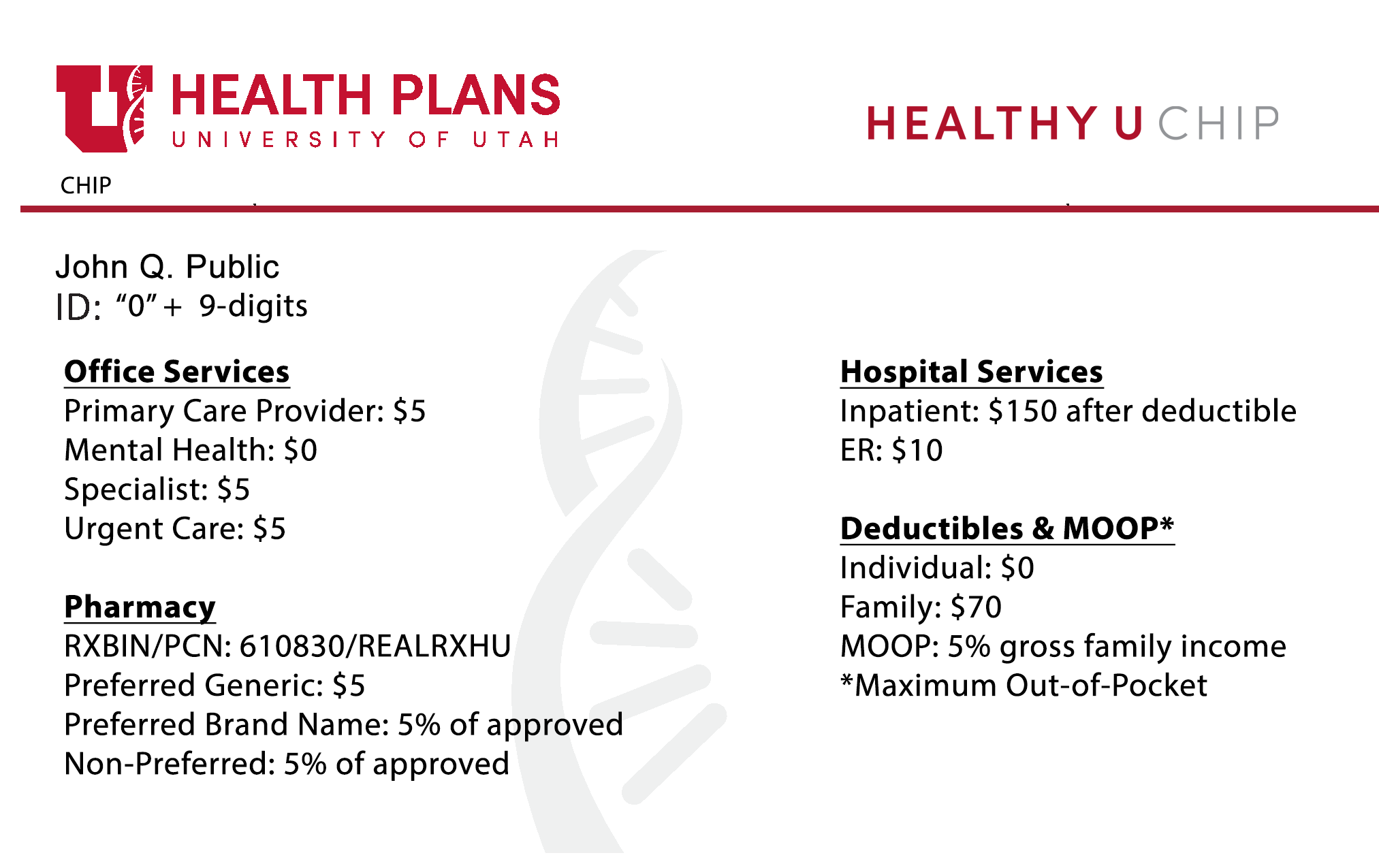
Healthy U CHIP
Healthy U CHIP plan name (CHIP A, CHIP B)
Healthy U CHIP is available to children who meet eligibility requirements for the Children’s Health Insurance Program (CHIP), provided they do not qualify for Medicaid or otherwise have health insurance. Member ID numbers consist of '0' followed by an additional nine (9) digits.
The Healthy U CHIP network provides coverage for Healthy U CHIP members.
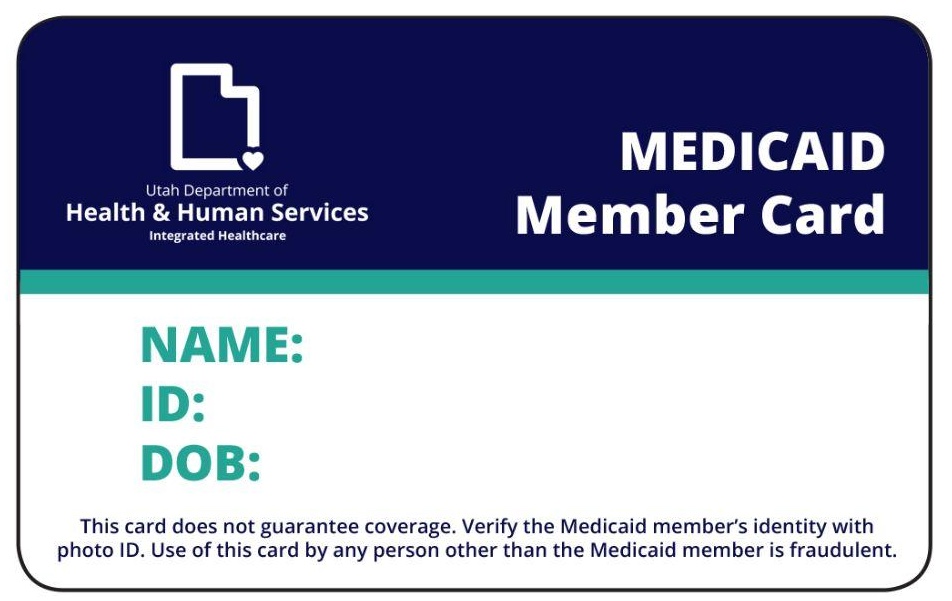
Healthy U Medicaid, Healthy U Behavioral, and Healthy U Integrated
Healthy U products include Healthy U Medicaid, Healthy U Behavioral, and Healthy U Integrated. These members should present their standard Utah Medicaid Identification card. Medicaid ID numbers contain 10 digits, beginning with 0 (zero). Because Medicaid eligibility can change from month to month, please verify eligibility prior to every visit via the Utah Medicaid PRISM Portal at prism.health.utah.gov.
Eligibility Questions?
Our secure Provider Portal offers up-to-date information regarding eligibility, benefits, prior authorizations, claims, payments, and more, 24/7.
Register or log in at uuhipprovider.healthtrioconnect.com
Support Contacts
- U of U Health Plans (Group): 833-981-0213 or 801-213-4008
- U of U Health Plans (Individual/Family): 833-981-0214 or 801-213-4111
- Healthy Premier U of U Hospitals & Clinics Plan (Employee): 833-443-3440 or 801-213-0274
- Healthy U Medicaid: 833-981-0212 or 801-213-4104
- Healthy U CHIP: 833-404-4300 or 801-213-0525
Appeals
Appeal Rights
- Advantage U (Medicare PPO) plans: Appeals must be received within 60 calendar days from the date of initial determination notification.
- Healthy U Medicaid: Appeals must be received within 60 days from the date on Notice of Action or EOB.
- Neurobehavioral HOME: Appeals must be received within 60 days from the date
on the Notice of Action or EOB. - U of U Health Plans Group, and Individual Plans Appeals: Members have 180 days to appeal from Notice of Action Letter/EOB.
- UNI & Miners: Please contact appeal coordinators at 801-213-4008 or 833-981-0213.
- Please note: Effective January 1, 2016, the University of Utah Health Plans will require that providers obtain consent from a Healthy U member to appeal on their behalf for denied claims or referrals relating to clinical services. A Clinical appeal means services that were denied in a pre-service review, or services that were billed and require medical review, that were denied.
File an Appeal
You, your legally authorized representative, or your provider may file your appeal. If you need help filing your appeal, call us at 801-213-4008. If you are deaf or hard of hearing, you can call Utah Relay Services at 711 or 1-800-346-4128.
Español: Si necesita esta carta en Español, por favor llamenos al 801-213-4008 o 1-833-981-0213 opcion 1. Si habla español, puede llamar a Spanish Relay Utah al 1-888-346-3162. Estos son servicios gratuitos de retransmisión telefónica pública o TTY / TDD.
Submission Information:
Send the complete written appeal to this address:
Appeals Team
6056 Fashion Square Dr., Suite 3104
Murray, UT 84107
Fax: 801-587-9985
Response Time
- Commercial: 45 calendar days.
- Medicaid: 30 calendar days.
If you or your provider believes your life or immediate health is in danger, you may ask for an expedited (quick) appeal by calling Customer Service at 801-213-4008. If we agree that the decision needs to be made quickly, we will make a decision in three calendar days for U of U Health Plans/Group and Individual Plans or 72 hours for Healthy U Medicaid.
For Routine or Expedited Appeals: Sometimes, we may need more information. If so, we may take an additional 14 calendar days to make our decision. If we need to take extra time, we will send you a letter. If you have U of U Health Plans Group or Individual Plans, we will contact you to explain why we need more time. We need your permission to take the extra time for the appeal review.
No Surprises Act: Requirements for Providers, Facilities, or Vendors
The No Surprises Act becomes effective January 1, 2022. This law represents a significant change in the way non-contracted and out-of-network providers can bill and be reimbursed by University of Utah Health Plans (U of U Health Plans). The Act prohibits balance billing of members by non-contracted and out-of-network providers for the following:
NOTE: For In-Network payment disputes, submit a payment dispute.
- Out-of-network emergency items and services.
- Covered medical items and services (nonemergency) performed by an out-of-network provider at an in-network HealthPartners contracted facility.
- Out-of-network air ambulance (rotary and fixed wing) items and services.
For each item or service identified with remark codes N859 and N860, the payment amount listed for each item or service is the Qualifying Payment Amount (QPA). The QPA applies for purposes of the recognized amount, or, in the case of air ambulance services, for calculating the applicable member cost sharing. Each QPA has been determined in compliance with the requirements of the No Surprises Act. Noncontracted providers may initiate a 30-day open negotiation period for purposes of determining the amount of total payment by contacting the U of U Health Plans Appeals Team to initiate open negotiation. You may initiate the No Surprises Act independent dispute resolution process within 4 days after the end of the 30-day open negotiation period if a determination of the total payment, including cost-sharing, is not reached.
To begin the Open Negotiation process, please submit the Open Negotiation Form to U of U Health Plans via:
- Email at: UUHP_Appeal_Compliance_Team@hsc.utah.edu
- Fax at: 801-587-9985
- Mail at:
- University of Utah Health Plans
Attention: Appeals Team
6056 Fashion Square Drive, Suite 3104
Murray, UT 84107
- University of Utah Health Plans
The parties must undertake an open negotiation period prior to initiating the Federal Independent Dispute Resolution (IDR) process and meet all timeliness requirements. Notification of IDR initiation should be submitted using the Notice of IDR Initiation (OMB Control No. 1210-0169 to the email, fax, or mailing address above.
Fraud, Waste & Abuse (FWA)
The University of Utah Health Plans is committed to detecting, preventing, correcting, and reporting suspected FWA behaviors, and will comply with all applicable state and federal laws, rules, and regulations.
What is FWA?
Fraud is the intentional deception or misrepresentation made by a person with the knowledge that the deception could result in some unauthorized benefit to them or some other person.
Examples of Fraud may include:
- Knowingly ordering medically unnecessary patient items or services
- Knowingly billing and/or documenting in the patient’s medical records, services of higher complexity than what were actually provided
Waste is the overutilization of services or other practices that directly or indirectly result in unnecessary costs to a state or federal healthcare program. Waste is generally not considered to be caused by criminally negligent actions, but rather the misuse of resources.
Examples of Waste may include:
- Conducting excessive office visits
- Ordering excessive laboratory or diagnostic tests
Abuse includes practices that are inconsistent with sound fiscal, business, or medical practices and result in unnecessary costs to the healthcare program. These practices include reimbursement for services that are not medically necessary, that fail to meet professionally recognized standards for healthcare, and recipient practices that result in unnecessary cost to the healthcare program (42 CFR 455.2).
Examples of Abuse may include:
- Billing for unnecessary medical services
- Charging excessively for services or supplies
What Are My Responsibilities?
You are a vital part of the effort to prevent, detect, correct, and report suspected FWA.
Comply with all applicable statutory and regulatory requirements, laws, regulations, policies, and guidelines.
- Bill for services according to what was provided, and follow proper coding guidelines.
- Ensure your data and billing are accurate and timely.
- Monitor and maintain accurate and complete medical records to ensure the documentation supports the services you rendered.
- Perform regular internal audits.
- Make sure you are up-to-date with the laws, regulations, guidelines, and policies.
- Be on the lookout for suspicious activity.
Follow your organization’s Code of Conduct that describes your commitment to standards of conduct and rules of ethical behavior.
- If FWA is detected, promptly correct it; develop an action plan to fix the underlying problem(s) that resulted in the FWA violation, to prevent future occurrences.
- Establish effective lines of communication with your colleagues and staff members.
Promptly report any violation of laws of which you may be aware.
How To Report Suspected FWA?
All entities, including contracted and non-contracted providers and staff, have a duty to report suspected FWA behaviors.
- Suspected FWA can be reported anonymously.
- When reporting suspected FWA, even if choosing to remain anonymous, always provide specific details and ensure all essential questions (who, what, where, why, and how) are addressed in the reporting form. Report suspected FWA by one of the following methods.
- U of U Health Plans FWA Email: HealthPlansReportFraud@utah.edu
- Online Form: Fraud & Abuse Reporting Form
- EthicsPoint Hotline: 888-206-6025 – Anonymity and interpretation services are available.
- EthicsPoint: secure.ethicspoint.com